We will soon be working on a project to explore priorities in pain research. To prepare for this, we wanted to get an overview of pain from the point of view of biomedical science, social science, and lived experience.
In this post, we’re sharing the most useful resources we came across and what we learned from them in case they might be useful for others interested in learning about this topic.
Textbooks
Textbooks are great for getting an accessible overview. We looked at a few and found this one most easy to engage with at this early scoping stage: Pain: A Textbook for Health Professionals. There is also Wall & Melzack’s Textbook of Pain which looked too detailed for getting started, and An Introduction to Pain and its Relation to Nervous System Disorders which was too advanced, although may become useful as we get deeper into the project.
Introductory pain science
We used a mix of YouTube videos and a textbook to familiarise ourselves with key concepts and processes.
The Science of Pain (and its Management) covers some of the basics of what pain is, types of pain, and types of drug treatments.
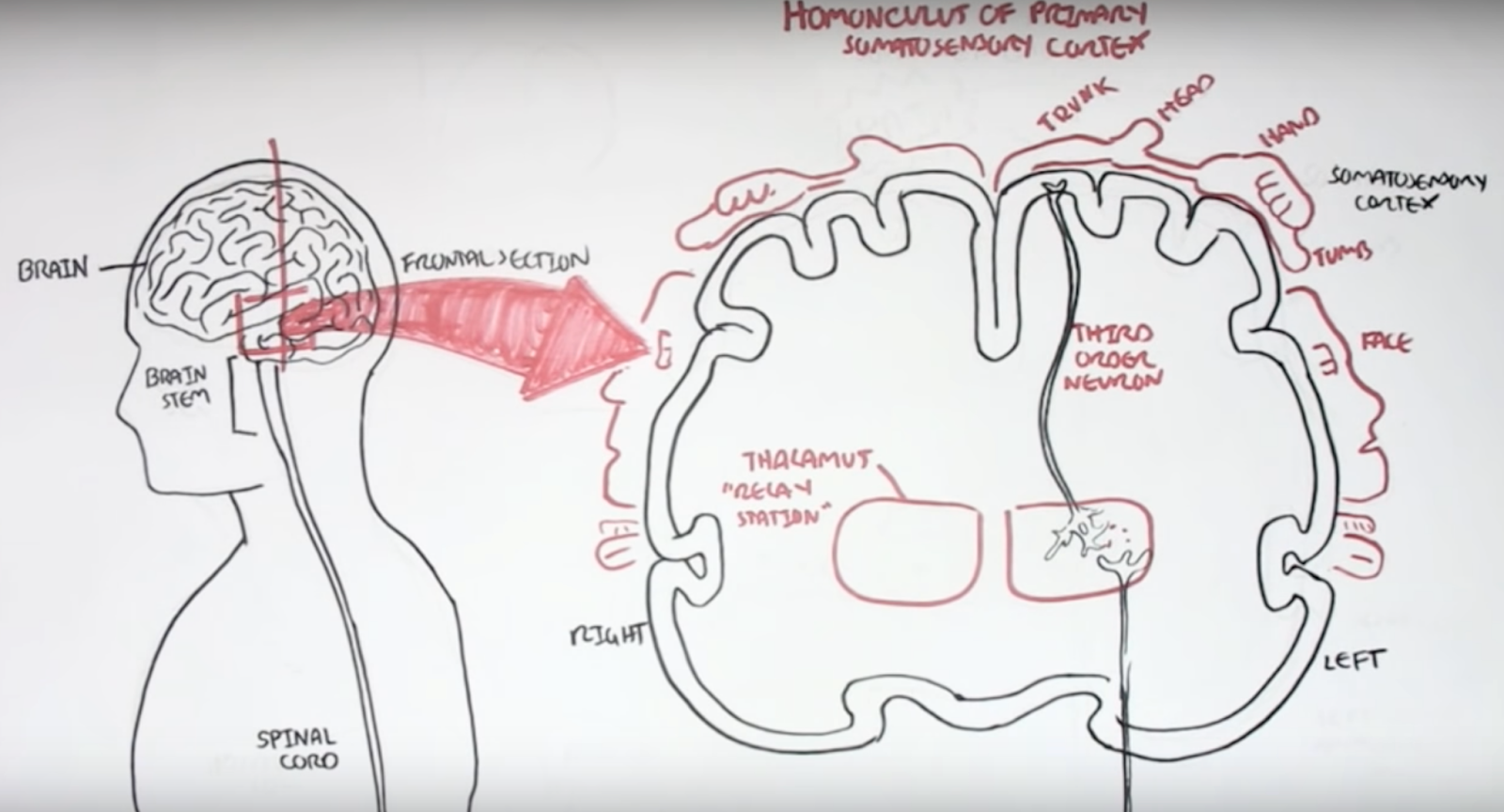
Armando Hasudungan creates videos with hand-drawn diagrams that are easy to learn from. His videos on nociceptors and pain physiology are useful starting points for pain specifically, and he has other videos on neurology such as Neurology - Divisions of the Nervous System.
Dr Matt & Dr Mike have an Introduction to Pain which is dense with clear, introductory information on biological mechanisms of pain and how pain drugs work.
Modern Brain and Pain Science and Implications for Care is an entertaining talk that describes a range of experiments in pain science, particularly on the psychological aspects of pain.
Finally, Section 1 (‘What is pain?’) of Pain: A Textbook for Health Professionals goes deeper on pain psychology, neuroanatomy, and neurophysiology.
Central sensitisation
We got interested in the role of central sensitisation in pain as it may explain how pain can become chronic. Central sensitisation “refers to the amplification of pain by central nervous system mechanisms.”1
We found this video to be an accessible starting point: Dr. Sletten Discussing Central Sensitization Syndrome (CSS). Then Chronic Pain and Sensitisation provides more detail on the biological mechanisms.
The neurobiology of central sensitization gives a detailed overview of the phenomenon. It was particularly interesting to learn about the overlap between different chronic pain conditions, many of which have been grouped under the term Chronic Overlapping Pain Conditions (COPCs), including fibromyalgia, irritable bowel syndrome, chronic fatigue syndrome, headache, endometriosis, and low back pain. It may be that all of these conditions have central sensitisation as an important cause. The article says that “many pain experts have suggested that COPCs are best understood as a single lifelong disease that merely tends to manifest in different bodily regions over time”.
The paper also makes a useful division between central sensitisation that is driven by ongoing input from pain sensors, and central sensitisation that has no such ongoing input. Which of these a patient has affects which kinds of treatment are likely to work.
Opioids
We wanted to find out more about opioids given their importance in managing pain and the challenges around the opioid crisis in the US.
A couple of resources helped us get oriented on biological mechanisms. Opioids and Opiates gives a brief introduction to the mechanisms by which opioids work and Opioids describes types of opioids, mechanisms, and adverse effects.
The Opioid Crisis: Past Present and Future is a short talk explaining the causes of the US opioid crisis and potential solutions. It outlines how well-intentioned goals such as listening to patients and taking pain seriously intersected with pharmaceutical company influence and financial incentives to create a problem of overprescription.
However, it’s important to realise that the swing away from opioids since then has caused significant problems in the US. Two articles in Wired describe the challenges that American chronic pain patients have in accessing opioids in the wake of the opioid crisis. In A Drug Addiction Risk Algorithm and Its Grim Toll on Chronic Pain Sufferers, they investigate software used throughout the US to help doctors and pharmacists to evaluate the risk of addiction in patients. How this software calculates its risk scores is opaque, but it has significant influence over prescribing decisions and this can lead to patients being denied medication that is essential for managing their pain.
[T]he most troubling thing, according to researchers, is simply how opaque and unaccountable these quasi-medical tools are. None of the algorithms that are widely used to guide physicians’ clinical decisions—including NarxCare—have been validated as safe and effective by peer-reviewed research.
In The Unseen Victims of the Opioid Crisis Are Starting to Rebel, Wired documents a movement of people with chronic pain campaigning for access to the opioids that they need.
The campaign to keep opioids away from people who abuse them has ended up punishing the people who use them legitimately—even torturing them to the point of suicide. Now they are pushing back, mobilizing as best they can into a burgeoning movement. “Don’t Punish Pain” rallies are taking place in cities nationwide on May 22, and pain patients are organizing a protest at the Centers for Disease Control and Prevention in Atlanta on June 21.
Lived experience
We also wanted to learn more about what it is like to live with chronic pain. Chapter 2 of Pain: A Textbook for Health Professionals gave a useful overview. It describes three ways that chronic pain affects people’s lives:
-
The search for restoration – people go through a long and frustrating process of trying to find a diagnosis and cure.
-
Loss – having chronic pain often leads to many difficult losses, such as loss of work, relationships, social roles, and valuable identities.
-
Stigma – people with chronic pain are often treated with suspicion by healthcare professionals and others in society.
The chapter also contains many quotes from people with chronic pain, which are valuable for understanding their experience. This is an excerpt from a quote by Ron:
I’m pretty stuffed I suppose, stuffed in many ways. The consequences of it are, I’ve lost my career, I’m a lousy father in the sense of my ability to handle the kids for more than an hour at a time, there’s no football, running on beaches, the ability to socialise, all those sorts of things I can’t do because movement aggravates pain, any movement aggravates muscle and joint pain. The fatigue denies me any ability to keep my brain alive, so going out to dinner and talking to someone is generally just not on.
We also discovered the healthtalk.org website which collects people’s experience of health conditions through video interviews. They have a section on chronic pain which covers people’s experiences of pain management, medication, and the impact of chronic pain on their lives. This site is particularly valuable as they use rigorous qualitative methods to develop their resources. This means, for example, that they work to represent a wide range of experiences of a condition.2
It was also useful to look at social media to understand more about people’s lives. There are many videos on YouTube where people with chronic pain talk about their experience. For example, this interview with someone with fibromyalgia or this Q&A by someone with trigeminal neuralgia and anesthesia dolorosa.
It’s also useful to read the comments on YouTube videos about chronic pain, as often people with lived experience will share their views. There are often many critical comments on videos of talks by researchers and doctors, which are useful for understanding some of the frustrations that people with lived experience can have with the medical system. Searching Twitter for chronic pain also brings up a lot of discussion.
We hope you found these links useful. If you are interested in learning more about our work in this space, or would like to share other useful resources, then do contact us via email or Twitter.
-
Harte, Steven E., Richard E. Harris, and Daniel J. Clauw. “The neurobiology of central sensitization.” Journal of Applied Biobehavioral Research 23.2 (2018): e12137. ↩
-
“To make sure that a wide range of experiences and views are included we use a method called purposive (or maximum variation) sampling (Coyne, 1997). We carry on collecting interviews until we are convinced that we have represented the main experiences and views of people within the UK” – Health Experiences Research Group ↩